The cancer drug that almost wasn't
Progress in cancer treatment can be frustratingly incremental. A new therapy often does no more than stall the disease by a few extra weeks. At a cancer meeting in San Diego, California, in April, however, University of California, Los Angeles (UCLA), oncologist Richard Finn reported that adding a drug called palbociclib to standard therapy doubled the time that women with metastatic breast cancer experienced no new tumor growth, from a median of 10 months to 20. “No study, despite efforts, has shown this dramatic improvement in progression-free survival, with the addition of a novel agent,” Finn told the audience.
The results won't dispel all doubts about the drug—or the new treatment strategy it represents. The phase II trial Finn discussed enrolled just 165 women, and it is too early to know whether those taking the drug combination live significantly longer than women on standard therapy. But palbociclib, which is under development by pharmaceutical giant Pfizer, has captivated the cancer field nonetheless. “The … buzz is that these are extremely impressive data that are really way beyond what anybody had expected,” says Frank McCormick, a veteran cancer researcher at UC San Francisco, who played an early role in the drug's discovery.
Palbociclib has traveled a long and tortuous road. The product of a project started in 1995 by researchers at Parke-Davis, a now-vanished drug company, the compound blocks key enzymes driving the cell cycle, the ordered set of processes by which a cell divides. Mounting scientific evidence suggested its potential in breast cancer. Yet Pfizer, where the compound was ultimately synthesized by the Parke-Davis team after Pfizer acquired their company, later shelved the then-unique drug for much of the decade. In the end, it took a handful of dedicated outside researchers to demonstrate its worth. Palbociclib “has reinvigorated the whole cell cycle area,” says Dennis Slamon, another UCLA oncologist involved in the breast cancer trial.
“Right now this looks like one of the bigger stories in the field for a long time,” adds Clifford Hudis, an oncologist at the Memorial Sloan Kettering Cancer Center in New York City and immediate past president of the American Society of Clinical Oncology (ASCO). He is excited not just by the potential of palbociclib to benefit women with metastatic disease, but also by plans to test it in early-stage breast cancer, where it might help cure patients. “That's a no-brainer.”
Clinical trials of palbociclib are under way in at least six other tumor types. And in June at ASCO's annual meeting, very similar drugs, from Novartis and Eli Lilly, showed excellent early results, often shrinking tumors or stabilizing them for long periods in people with melanoma and lung cancer. “The implications of this [drug] class will be wide,” predicts Thehang Luu, an oncologist at the City of Hope cancer center in Duarte, California. “We're not even touching the surface yet.”
THE SPECIAL APPEAL OF palbociclib and its competitors lies in the nature of the cell cycle. Targeted cancer therapies such as Herceptin and Tarceva interrupt one strand of a weblike network of growth signals within the cell, but it's hard for a single drug to overcome multiple, redundant signaling pathways and feedback loops. But the cell cycle is not a web; it's a one-way street. So blocking any component should, in theory, stop the frenetic cell division of cancer cold.
Dividing human cells cycle through four distinct phases, known as G1, S, G2, and M (for mitosis). Experiments in the 1970s and 1980s in three different organisms revealed this cycle's key molecular components and earned Leland Hartwell, Tim Hunt, and Paul Nurse the 2001 Nobel Prize in physiology or medicine (Science, 19 October 2001, p. 502). Proteins called cyclins and cyclin-dependent kinases (CDKs) lock together and drive each step of the cycle. By 1995, there was strong circumstantial evidence that cyclin D and either CDK4 or CDK6—the complex that triggers human cells to move from G1 to S (see graphic, p. 867)—often drives uncontrolled cell division and tumor growth.
“Even back then it was pretty clear [that] different components of this pathway are mutated, or altered in some way or another, in the majority of cancers,” says UC San Francisco's McCormick. That made the CDK4/6 system an obvious target for inhibitory compounds. In 1995, Parke-Davis, the pharmaceutical research arm of health care company Warner-Lambert, approached McCormick, the founder of Onyx Pharmaceuticals, to collaborate. Work began that year at the Parke-Davis labs in Ann Arbor, Michigan. Investigators used lab-made versions of CDK4 and other cell cycle proteins, supplied by Onyx, to guide discovery of compounds that specifically inhibit CDK4.
Because the many CDK family members are almost identical, “creating a truly selective CDK4 inhibitor was very difficult,” says former Parke-Davis biochemist Dave Fry, who co-chaired the project with chemist Peter Toogood. “A lot of pharmaceutical companies failed at it, and just accepted broad-spectrum CDK inhibitors as their lead compounds.” But after 6 years of work, the pair finally succeeded with the help of some clever screens that could quickly weed out nonspecific “dirty” compounds.
Their synthesis in 2001 of palbociclib, known internally as PD-0332991, was timely. By then, many dirty CDK inhibitors from other companies were already in clinical trials, but they worked poorly, if at all. Because they hit multiple CDK targets, these compounds caused too much collateral damage to normal cells. “They had a lot of toxicity,” Slamon notes. That made it hard to give these drugs at the doses necessary to shut down the cell cycle in tumors. It soon also became clear that the cell cycle had some built-in redundancies of its own, leaving many to wonder if taking out a single component would really stop a tumor in its tracks. Eventually, most efforts to fight cancer by targeting the cell cycle ground to a halt. “Everything sort of got hung up, and I think people lost enthusiasm,” Slamon says.
PD-0332991 fell off the radar screen. Pfizer, which had acquired Warner-Lambert/Parke-Davis in 2000 mainly for the cholesterol drug Lipitor, did not consider the compound especially promising, Fry says, and moved it forward haltingly at best. “We had one of the most novel compounds ever produced,” Fry says, with a mixture of pride and frustration. “The only compound in its class.”
A major merger helped bury the PD-0332991 program. In 2003, Pfizer acquired Swedish-American drug giant Pharmacia, which flooded Pfizer's pipeline with multiple cancer drugs, all competing for limited clinical development resources. Organizational disarray followed, says cancer biologist Dick Leopold, who led cancer drug discovery at the Ann Arbor labs from 1989 to 2003. “Certainly there were some politics going on,” he says. “Also just some logistics with new management and reprioritization again and again.” In 2003, Pfizer shut down cancer research in Ann Arbor, which left PD-0332991 without scientists and managers who could demand it be given a chance, Toogood says. “All compounds in this business need an advocate.”
Pfizer finally launched a phase I human trial in 2004 to establish a safe dose for PD-0332991. Typically, drug developers start phase II trials about a year later, but Pfizer did not follow up. In a statement, the company notes that the drug failed to show much antitumor effect in the phase I trial. But Fry and Toogood say the trial was inadequate. Patient selection was “essentially solid tumor, all comers, looking for a signal,” Toogood says. “That's a tough way to get really exciting data on a compound as targeted as this is.” Fry says that Pfizer could have tracked biomarkers in patients' tumors showing whether palbociclib was having its desired effect. And, he says, it could have monitored alterations in the CDK4 system that could later be used to predict who would benefit from the drug. Pfizer has stated that the biological knowledge to predict responses back then was lacking and says, “We have moved rapidly and responsibly, utilizing emerging evidence, to advance the clinical development of palbociclib.”
But a phase II trial of the drug did not start until 2009, 5 years after the phase I study. By then, strong genetic evidence already existed that certain breast tumors are completely dependent on CDK4. Piotr Sicinski, a geneticist at the Dana-Farber Cancer Institute in Boston, reported in 2001 in Nature that mice lacking cyclin D1 (CDK4's partner) cannot develop breast cancer driven by the Ras or Her2 oncogenes. “Unfortunately this study went unnoticed to the pharmaceutical industry,” says Mariano Barbacid, a cancer researcher at the Spanish National Cancer Research Center in Madrid.
Then, in January 2006, Sicinski reported in Cancer Cell that mice needed CDK4 as well as cyclin D to develop breast tumors. In an accompanying editorial, Barbacid and a colleague acknowledged that human tumors are more genetically complex than Sicinski's mouse models, but wrote that “these considerations should not be an excuse to further delay testing in patients suffering from … breast tumors the effectiveness of selective Cdk4/6 inhibitors.” But the only such drug, Pfizer's, remained on the shelf.
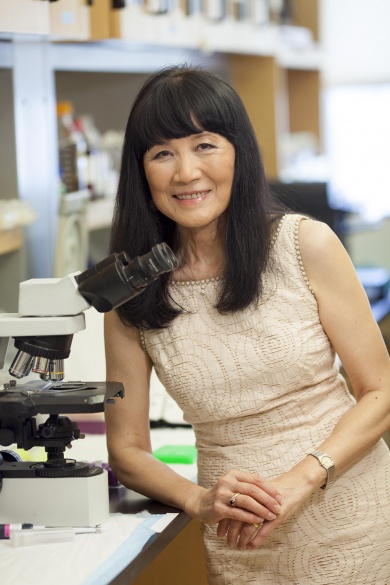
IN THE END, PD-0332991 WAS resurrected by investigators outside the company. In late 2004, Selina Chen-Kiang, a molecular biologist at Weill Cornell Medical College, obtained PD-0332991 from Pfizer as a research tool for studying the cell cycle in normal immune cells. Convinced of the drug's potential in blood cancers, she persuaded Pfizer to sponsor a 17-patient phase I clinical trial in mantle cell lymphoma that began in 2007. In that trial, about one-fifth of patients had significant tumor shrinkage—decent but not spectacular results. Still, Toogood says, “her advocacy was important in helping ensure that the program continued.”
In May 2007, Slamon, whose earlier research had led to the breast cancer drug Herceptin, applied PD-0332991 to a large panel of breast cancer cell lines. Slamon expected the cell cycle inhibitor to work best in aggressive “triple-negative” tumor cells, which proliferate rapidly, but to his surprise estrogen receptor (ER)–positive lines were most sensitive. More than 60% of all breast cancers are ER-positive.
Slamon and UCLA's Finn then tested PD-0332991 in combination with letrozole, a standard antiestrogen, in a dozen women with ER-positive metastatic breast cancer. Three of the women had at least 30% tumor shrinkage. “That encouraged us even more,” says Slamon, who says that one woman is still taking the combination treatment more than 4 years later.
At this point, Pfizer got excited, too. It sponsored the randomized phase II trial, which involved UCLA and other medical centers internationally and started in December 2009. While awaiting proof that the drug improves overall survival, Pfizer announced this week it has asked the Food and Drug Administration to approve the drug for ER-positive metastatic breast cancer, based just on the phase II results—the agency has designated it a “breakthrough therapy,” earning it priority for evaluation. Yet both Sloan Kettering's Hudis and Martine Piccart, a breast cancer researcher at the Jules Bordet Institute in Brussels, say that results from a larger, phase III trial are necessary to really know palbociclib's worth. Two phase III breast cancer trials have completed patient enrollment, and others are under way.
On the basic research side, scientists are still seeking to explain an unexpected bonus: palbociclib's ability to shrink tumors. In theory, a cell cycle inhibitor should only stop a tumor from growing. And that, indeed, is what happens in cancer cell lines. But, back in 2001, at the Ann Arbor labs, the drug completely eradicated human colon tumors transplanted into mice. “That was a very exciting result,” Toogood recalls.
In the clinic, one lymphoma patient taking just palbociclib early on had a complete remission, and dozens of breast cancer patients have seen their tumors shrink. Lilly's CDK4/6 inhibitor, given alone, has also shrunk both breast and lung tumors. “The phenomenon is real,” Slamon says. “And we're left to explain it.”
Mouse studies suggest one possibility. Eliminating the genes encoding CDK4 in a rodent—a process that palbociclib roughly mimics—can put its cells into senescence, a permanent inability to divide. Such senescent cells may ultimately be cleared by the immune system, leading to tumor shrinkage. In addition, Chen-Kiang has data from human tumor tissue showing that the prolonged cell cycle arrest by palbociclib makes the tumor cells highly vulnerable to other cancer drugs. And, in a few animal models of leukemia and lymphoma, the drug causes tumor cells to commit suicide.
Cancer cells are notorious for their ability to develop drug resistance. But investigators suspect resistance to palbociclib and other CDK4/6 inhibitors may be slow to arise; initial studies of people taking the drugs have so far shown no evidence that their tumors acquire mutations in the genes for the CDKs. CDK4 and CDK6 “are extremely stable drug targets,” Chen-Kiang says. Still, some studies of cells dosed with palbociclib suggest that resistance can develop indirectly, if the cells lower amounts of a negative protein regulator of the cell cycle, for example.
Pfizer leads the race for the first approved CDK4/6 inhibitor, but its sluggish development gave competitors time to catch up. Novartis and Lilly already have their compounds in phase III trials in breast cancer, and Lilly will soon start a phase III trial of its drug in lung cancer. Both companies apparently identified their compounds only about 5 years ago, almost a decade after Fry and Toogood found palbociclib.
But thanks to their drug, the cell cycle is again a hot field for cancer research. The ultimate payoff on palbociclib or its competitors remains anyone's guess. “If we don't really know why they work so well, quite frankly, it's quite difficult to predict the impact overall,” McCormick says. “I would guess it's just the beginning of a whole new era of developing this approach to targeting cancer. But how far it'll go, I really couldn't say.”
This article first appeared in the August 22 issue of Science