Some pediatric regimens can be successful in adults with ALL
When Jody Winsick-Soluri was diagnosed with acute lymphoblastic leukemia (ALL), she found out she had a chromosomal abnormality, the Philadelphia chromosome, which made her prospects bleak.
“I was bleeding out; they said I might only have 24 hours to live,” Winsick-Soluri remembers.
Now, after many rounds of chemotherapy, total body irradiation, two bone marrow transplants and seven years, Winsick Soluri takes a targeted drug — Sprycel (dasatinib) — that blocks a protein leukemia cells need to proliferate.
“Now, I’m four-and-a-half years out from the last transplant,” the New Jersey mother of four says. “More people with ALL are staying alive a lot longer.”
Jeremy Katzman was 21 and a junior at the University of Florida when he was diagnosed with ALL. Though technically an adult, Katzman’s medical team suggested that he undergo a longer, more aggressive pediatric protocol to treat his disease, a new idea at the time. Twelve years later, he’s disease-free.
“I’m glad I did it. Knock on wood, I’m doing OK,” says Katzman, now 33 and the father of a toddler.
Leukemia became the first great success story of cancer treatment when the earliest chemotherapy drugs were used to treat children with the disease in the late 1940s. Since then, new chemotherapy drugs and regimens have developed, but the basic idea behind the treatment — several long courses of aggressive chemotherapy — has remained largely the same, experts say. So has the general separation between pediatric cases of ALL and adult cases, both in research and in treatment.
Because of patients like Winsick-Soluri and Katzman, however, those lines are beginning to blur. Experts say we are now poised to investigate the biology of ALL across an age spectrum from 1 to 50.
At the Dana-Farber Cancer Institute, for instance, there is a combined Adult- Pediatric ALL Consortium; similar groups are convening worldwide. Adults — for whom a typical past strategy was to take chemotherapy until their disease was well enough controlled for a bone marrow transplant — may now follow programs inspired by pediatric treatment: several courses of intense chemotherapy that may go on for two to three years. And other teams are beginning to better understand the biology of ALL, using therapies that enlist the patient’s immune system and targeted agents like the one that makes such a difference for Winsick-Soluri.
“I think it’s an exciting time now. Several things are happening: Our knowledge of the biology is improving, and also the technology. We are developing new ways of treating ALL, and specialists in pediatric and adult ALL are working together much better,” says Dr. Sima Jeha, a pediatric ALL specialist at St. Jude Children’s Research Hospital in Memphis, Tennessee.
UNDERSTANDING ALL
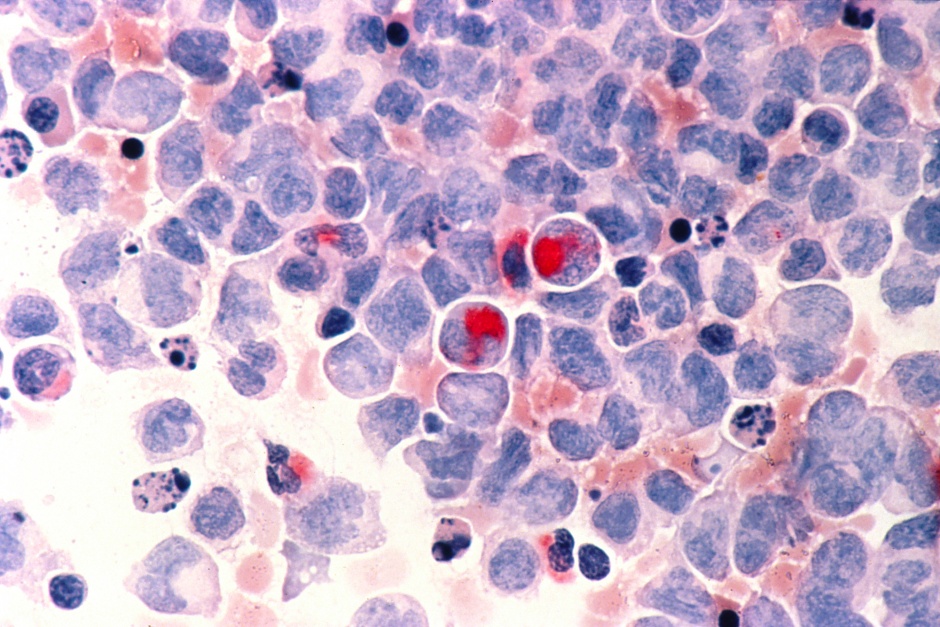
ALL is an aggressive type of leukemia characterized by a rapid growth of lymphoblasts that take over the blood-making bone marrow, and commonly enter the bloodstream as well. A lymphoblast is an immature cell that has the potential to develop into several kinds of white blood cells: plasma cells that help transport nutrients, hormones and proteins around the body, as well as T lymphocytes and “natural killer cells” that make up part of the body’s immune system arsenal. However, in ALL, the lymphoblasts do not mature to develop into these specialized cells.
As is the case with many cancers, experts are learning that ALL isn’t really a single disease. It seems, instead, to be a group of related diseases with different biomarkers and subtypes. Treatment and prognosis can vary widely depending on subtype, age, each individual’s reaction to treatment and other factors.
“ALL is not one disease, it’s a cluster of diseases,” says Jeha. “It varies with age, with subtypes, and you need to tailor the therapy to make it personalized and directed. It’s not one size fits all.”
“There appear to be complex biological differences between pediatric and adult ALL, and we are just starting to unravel these in the laboratory. Hopefully, we can exploit the different mutations, signaling pathways and surface antigens as druggable targets. Even knowing that, we don’t fully know what the answer is,” explains Gail Roboz, M.D., professor of medicine and director of the Leukemia Program at Weill Cornell Medicine.
....
This is an excerpt of an article that appeared in CURE Magazine. Read the full feature here.