Researchers decode role of leading mutated gene in cancer
A genetic mutation implicated in a common and incurable form of non-Hodgkin lymphoma drives disease development by disrupting the mechanism that manages normal immune cell growth, according to new research led by investigators at Weill Cornell Medical College and Memorial Sloan Kettering Cancer Center. The finding may explain why this lymphoma subtype becomes treatment-resistant, and may also open the door to new therapeutic strategies for this and other types of cancer.
Investigators previously discovered through genomic sequencing that 80 percent of follicular lymphoma cases have mutations that disrupt KMT2D gene, but little was known about how that gene factored into cancer development and growth. In a study, published Sept. 14 in Nature Medicine, an international research team found that KMT2D is required for B-immune cells to properly function, generating antibodies against invading microbes.
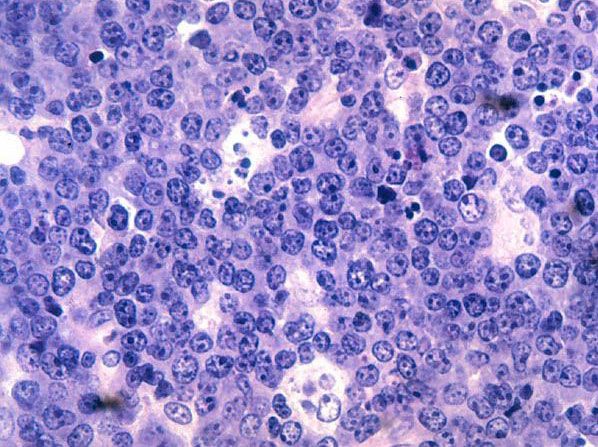
The research team found that normally KMT2D prepares key genes to respond to signals from other immune cells that stop B-cells, also called B-lymphocytes, from dividing and cause them to start making antibodies. However, when KMT2D mutations develop in B-cells, these external signals are no longer able to restrain them from dividing and stimulate their production of antibodies. As a result, there is an accumulation of rapidly dividing B-cells that eventually become malignant lymphomas. Importantly, the group demonstrated that therapies that have been developed to kill lymphoma cells by targeting these same signals are ineffective in the presence of KMT2D mutations.
"KMT2D turns out to be one of the top 20 most mutated genes across all cancer types. It is really one of the superstars of cancer because it is one of the genes that is most strongly linked to tumors," said co-senior author Dr. Ari Melnick, chair of the hematologic malignancies program in the Sandra and Edward Meyer Cancer Center and the Gebroe Family Professor of Hematology/Oncology at Weill Cornell Medical College. "Now that we understand how the gene functions in this treatment-resistant lymphoma, we can investigate the role of KMT2D mutations in other cancer types."
"We think that understanding the molecular causes of complex diseases like lymphoma is an important step towards new and better therapies," said Dr. Hans-Guido Wendel of the Cancer Biology and Genetics Program at Memorial Sloan Kettering. "For example, emerging new drugs are able to target some of these signaling pathways and may be effective against these tumors."
KMT2D is a member of a small family of proteins that can chemically modify a specific amino acid on proteins around which DNA is wrapped, called histones. Using fruit flies, other investigators had previously shown that KMT2D marks a specific amino acid on a particular histone located in areas of the genome that had been called junk DNA — but which are now known to be biologically active.
KMT2D is an epigenetic regulator, Dr. Wendel said. These regulators do not affect gene structure, but can change gene expression. When KMT2D marks histone 3 on the amino acid, the nearby genes are in turn made accessible to signaling proteins that are supposed to turn them on. When disrupted by KMT2D mutation, the "loss of this subtle histone change consequently reduces activity of several hundred genes," he said. "Importantly, the genes that are especially affected by this mechanism are among the most critical factors of normal lymphocyte behavior and growth control."
As a result, defects in KMT2D re-program lymphocytes, leading to development of lymphomas, the scientists say. Upon an immune attack, B cells quickly create a variety of antibodies until they produce one with the perfect structure to latch on to a unique molecule on the offending microbe, tagging it, or an infected cell, for destruction. When that antibody is created, KMT2D helps turn on the molecular switches in the junk DNA portion of the B cell's genome that will tell the B cell that it is done. The defective gene prevents that process from happening, enabling B cells to grow unabated.
Dr. Melnick likens the process to chefs in a Michelin-starred restaurant "cooking a giant pot of soup, and they keep stirring until someone tastes it and says the soup is perfect," he said. "But imagine what happens if the person who tells the chefs to stop cooking can't talk to them anymore — can't get through. The chef keep cooking, and that is what you have when KMT2D is mutated. If B cells can't receive the signal to stop, they will keep dividing and will transform into malignant lymphomas."