Target Practice: Precision approaches are a major advance in the treatment of blood cancers
As chief executive of a New Jersey-based global food importer, George Gellert works hard and plays hard. But two summers ago, during his regular tennis game, something felt off. "All of a sudden, my energy was zapped," says Gellert, who's in his mid-seventies. He didn't think it was serious, but he went to his doctor anyway — and when the blood test results came back, the physician didn't like what she saw. After being referred to Weill Cornell hematologist-oncologist John Leonard, M.D., he got the diagnosis: lymphoma.
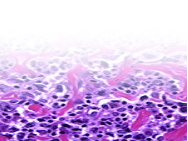
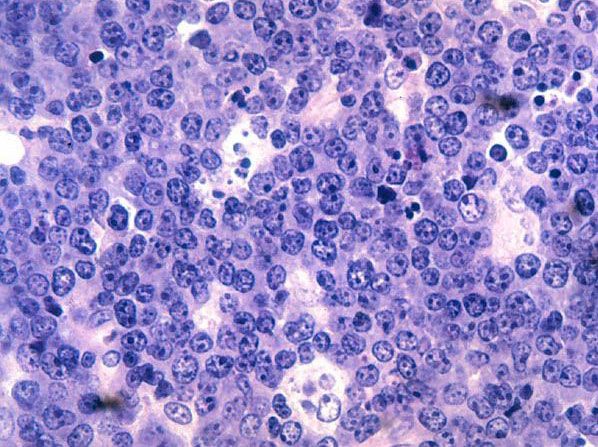
For many patients receiving such news, that's the only word they remember hearing. Lymphoma, a blood cancer in which tumors form in the immune system, kills some 20,000 Americans a year. Like many cancers, however, lymphoma is not a single disease but a diverse group of malignancies. Originating in the immune system's white blood cells known as lymphocytes, it consists of two main types — Hodgkin's and non-Hodgkin's (NHL). Within those two forms, more than sixty subtypes have been categorized based upon pathology — whether it originates from B-cells or T-cells, aggressive or indolent, and so on. When molecular characteristics of tumors are factored in, subtypes get divided even further. No two tumors, in fact, may be alike.
This diversification of what was once considered a singular disease defines a striking new approach to cancer research and treatment at Weill Cornell's Sandra and Edward Meyer Cancer Center and elsewhere. Leonard, associate dean for clinical research and the Richard T. Silver Distinguished Professor of Hematology and Medical Oncology, notes that for many years, most lymphomas had been treated the same way. "It was kind of one size fits all,” he says. "But it didn't fit very well." Today, therapies are increasingly being tailored to the personal characteristics of patients and their cancers. "You shouldn't treat everybody who walks in the door the same way," says Leonard. "We want to treat with a tailored approach based on what's most likely to work for that individual patient."
"You shouldn't treat everybody who walks in the door the same way. We want to treat with a tailored approach based on what's most likely to work for that individual patient."
Leonard stresses that it's not particularly helpful to identify subsets of patients if you don't have the tools to treat them differently. For Gellert, the specific diagnosis was diffuse large B-cell lymphoma (DLBCL), the most common type of lymphoma and a highly aggressive form. With chemotherapy, DLBCL is curable in about two-thirds of cases — but for the remaining third, it either does not respond to chemo or does only briefly before relapsing. Patients who fall into the latter category, many of whom are elderly, typically die within two years of diagnosis. This makes refractory, or resistant, DLBCL one of the greatest unmet needs in lymphoma treatment, says Leonard. Given Gellert's age and other characteristics, he gave him a roughly 50 percent chance of a cure with standard therapy. As Gellert puts it dryly: "I didn't like that."
Blood cancers have been at the forefront of research on tailored approaches to treatment, known as precision medicine. In large measure, these advancements are due to researchers' ability to access tumor material from such patients more readily than they can with other types of cancer. In the past decade, Weill Cornell researchers have been involved in developing or testing almost every new lymphoma drug recently approved by the FDA. While most cancers today are treated primarily through surgery and radiation, Leonard notes, cancers of the blood are different. "Lymphoma is a disease where treating with drugs is central to curing the patient," he says.
The promise of creating that next generation of medications is what motivates Ari Melnick, M.D., the Gebroe Professor of Hematology and Oncology and director of the Raymond and Beverly Sackler Center for Biomedical and Physical Sciences. He began his career as a clinician, but gradually moved to the laboratory full time. "I was frustrated with chemotherapy and didn't feel it was really the answer," Melnick says. "I felt I could have a greater impact in the lab in terms of developing more definitive drugs."
"Now we know that when considering tumors, one has to take into account that both the genome and the epigenome are equally important parts of the instructions that govern cells.'
Lymphomas are also ideal candidates for targeted therapies because, as researchers are increasingly learning, they are highly subject to epigenetic regulation — the chemical modifications that determine how cells behave. Every cell in the body is governed by a set of instructions, found in both the genome and epigenome. Melnick uses the analogy of a computer, likening the genome to hardware — the components that come with the system — and the epigenome to software, which actually determines what functions the computer can perform. Known as the regulatory genome, the epigenome is a form of chemical coding, independent of DNA sequence, which controls the various functions of the genome including the regulation of all genes. Says Melnick: "Now we know that when considering tumors, one has to take into account that both the genome and the epigenome are equally important parts of the instructions that govern cells."
Studying patients with acute myeloid leukemia, Melnick developed epigenome maps of human tumors and found that regulation of the epigenome is a hallmark of the disease. "We've developed methods to read these epigenetic instructions in patient tumor cells," he says. "Then we've used that as a kind of blueprint to map out which master regulators might be writing those instructions." With the aim of preventing these regulators from writing cancer-causing instructions into the cells, researchers want to understand how they work from a biochemical standpoint and then develop drugs that block their activities.
After Gellert's diagnosis, he prepared himself for six rounds of chemotherapy, knowing he had a fifty-fifty chance that it would work. But just a few days before treatment was to start, he got a call from Leonard. The oncologist told him about a new proof-of-concept Phase 1 clinical study led by Peter Martin, M.D., assistant professor of medicine and the Charles, Lillian, and Betty Neuwirth Clinical Scholar in Oncology. Should Gellert enroll, Leonard told him, for approximately one week before his chemotherapy began he'd take azacitidine, an existing drug approved for treatment of myelodysplastic syndrome. "I told him, "I'm game," Gellert recalls. "I was the ninth patient to take this regimen."
The protocol was based on the work of Leandro Cerchietti, M.D., assistant professor of medicine and the Raymond and Beverly Sackler Research Scholar. Cerchietti's team had discovered epigenetic aberrations in DLBCL tumors that were resistant to chemotherapy — mutations that prevented certain genes from being expressed and made the tumors more aggressive. Cerchietti turned to azacitidine, a known methyl transferase inhibitor, to see if it would reverse the epigenetic process that was silencing the gene — and if so, restore the chemotherapy's ability to kill cancerous cells. One of the most common forms of epigenetic alteration is methylation, the process by which a methyl group, consisting of three hydrogen atoms and one carbon, attaches to DNA and switches off the gene. Cerchietti and his team discovered that the cells of DLBCL tumors had a high degree of DNA methylation, which was making them resistant to chemotherapy. These methyl groups, also known as silencing chemicals, were preventing tumor cells from dying by inactivating genes that normally suppress tumor growth.
At first, the researchers tried administering high doses, but found it damaged DNA, which caused other effects. At low doses, however, the drug allowed for re-expression of the genes that had been shut down without causing damage. Once the broken pathways were reactivated, the resistant cells were vulnerable to chemotherapy. "In essence," says Cerchietti, "we're reprogramming the cancer into a more benign tumor." And by uncovering an important weakness in the tumor and finding a way to exploit it with an existing drug, the researchers and oncologists were able to get new therapies to patients in need very quickly.
Gellert received three injections of azacitidine per day for five days in the week before beginning chemo. (The drug is now being tested in oral form.) When Cerchietti and his colleagues published the trial results in Cancer Discoverylast summer, Gellert was among the ten out of twelve patients who'd remained cancer-free for up to twenty-eight months. In addition to the high rate of complete remission, the therapy was well tolerated.
Cerchietti is testing the approach against other aggressive lymphomas, as well as advising teams at Weill Cornell and elsewhere that are taking the same approach in solid-tumor cancers such as those of the breast, lung, and colon. For the next trial, oncologists will prolong the duration of azacitidine treatment to ten days, thus allowing more time for a complete lymphoma reprogramming. Over the course of treatment, Cerchietti's team will monitor changes in gene expression through a simple blood draw. "The ultimate goal is to administer the drug until you get the maximum reprogramming effect," he says. "No more, no less."
Leonard notes that the precision medicine approach is inherently challenging; smaller subsets of patients can make it difficult to build large cohorts for clinical trials. But the molecular characteristics of cancers that scientists are revealing have totally changed the game, Melnick says, making the field of blood cancer research unrecognizable from just a few years ago. "Thanks to critical insights and new technology, we're able to advance at a speed that is far beyond what I ever imagined," he says.
With almost 90,000 new cases of lymphoma estimated to be diagnosed this year, speed in the laboratory and the approval process translates into saving lives. Gellert, for one, is grateful he had the chance to be treated under the new paradigm. "I got sick in July," he says, "and in December I was skiing."
MASTER CLASS: TAKING AIM AT THE "UNDRUGGABLE"
The epigenome — a.k.a. the regulatory genome — is controlled by master regulatory proteins called transcription factors. Each of these master regulators controls thousands of genes within cells. One such factor is the protein BCL6 — and from the time Ari Melnick, MD, started his lab, he's been studying it.
Expressed in nearly all types of B-cell lymphomas, BCL6 is required for the development and survival of diffuse large B-cell lymphoma (DLBCL). But it also plays a role in maintaining the healthy function of many immune cells, so to disable it entirely could bring about severe side effects, including systemic inflammation and atherosclerosis.
For years, master regulators like BCL6 have been considered "undruggable" too complex to target. BCL6, for example, works largely through protein-protein interactions rather than enzymatic activities — which have long been the standard targets of pharmaceutical development. Master regulators had not been considered in the past, Melnick says, because scientists didn't understand how they work. "These master regulatory factors are present in the cell nucleus and bind directly to DNA," he explains. "Some are brought to DNA by other kinds of molecules. So there are very different scenarios for how these instructions are rewritten."
Melnick, the Gebroe Professor of Hematology and Oncology and director of the Raymond and Beverly Sackler Center for Biomedical and Physical Sciences, and his team at the Sandra and Edward Meyer Cancer Center have made a number of observations about BCL6's partner proteins and how it interacts with them at the structural level. They have mapped out which atoms on the proteins interact with each other and found that BCL6 functions as a kind of "Swiss army knife" — using certain partner proteins for its effects in cancer and others for its actions in the immune system and inflammation. Based on these results, Melnick developed a new class of drugs that only specifically block the effects of BCL6 in cancer without affecting its role in controlling inflammation. "With that, we've been able to achieve success in designing drugs that target the undruggable," he says. "We can block the lymphoma functions of BCL6 without affecting its other actions in normal tissues, so we can hit BCL6 in tumors without having a toxic effect on normal cells."
Melnick's lab developed a novel therapy to target that site on BCL6; last fall, in a study published in"Cell Reports, it showed that five doses of the drug eradicated human lymphoma in mice — with no other form of treatment or any discernible side effects. He and his colleagues are refining these drugs so they can be tested in clinical trials. What's more, the protein appears to be active in a number of other cancers; collaborators around the country have found Melnick's new inhibitor to be powerful in killing lung and breast cancer cells.
This story first appeared in Weill Cornell Medicine, Vol. 13, No. 2.