Tumors' mechanical properties affect protein production
Tissues stiffen with age, poor diet, disease and for natural reasons, and when they do, a new study shows, proteins produced by such cells can be altered, which in turn affects downstream processes.
The finding, published June 23 in the journal Proceedings of the National Academy of Sciences, provides new ways for scientists to promote or limit the production of certain proteins through a tissue’s softness or firmness, and opens doors to develop tumor-fighting drugs and tissue engineering.
The fundamental discovery applies to any instance where tissues stiffen, such as in atherosclerosis, diabetes, wound healing and embryonic development where mechanical properties of tissues change continuously.
“It’s a general universal phenomenon that when given this stiffer environment, cells change how they produce proteins,” said Cynthia Reinhart-King, Ph.D., an associate professor of biomedical engineering and the paper’s senior author. Francois Bordeleau, a postdoctoral associate in Reinhart-King’s lab, is the paper’s lead author.
Tissue stiffness refers to a tissue’s hardness or softness. “There’s some clinical data to show that stiffer tumors, such as denser breast tumor tissue, are more likely to be aggressive,” Reinhart-King said.
Cells use a mechanism called alternative splicing to diversify proteins they produce. In the presence of stiffer tissue, this study shows, cells adapt to the new environment by splicing out certain sections of proteins they produce, chopping off a tail, front end or middle section of a protein. When the form of a protein changes, it can often change its function, how it will interact or where it ends up in a cell, said Bordeleau.
“Tumors have a number of alternatively spliced proteins that only exist in tumor tissue and exist very few other places,” said Reinhart-King. One of these is a protein called extra domain B-fibronectin (EDB-FN), whose role is not yet clear, but because it is tumor-specific, drug companies and researchers have suggested it would be a good target for a drug delivery vehicle that binds to EDB-FN and delivers a therapy locally and specifically to tumor tissue.
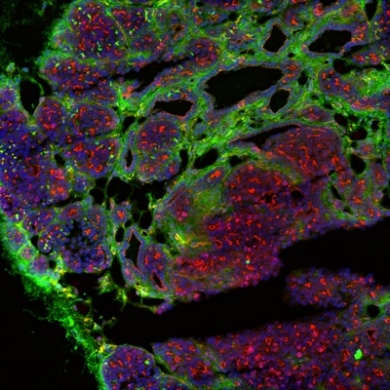
Apart from EDB-FN, the researchers looked at two other cell proteins that are alternatively spliced due to stiffening tissue in tumors. One of these proteins is vascular endothelial growth factor, or VEGF, which is important for triggering blood vessel growth in the tumor. Proliferation of blood vessel growth into solid tumors is essential for tumor growth, Reinhart-King said.
“As the stiffness increased, we can see the emergence of a spliced version of VEGF that is most potent for up-regulating angiogenesis” or blood vessel growth, Bordeleau said. “In fact, it brings down a version of VEGF that blocks angiogenesis.”
While it has been known that proteins can be alternatively spliced, and certain chemical signals mediate those splices, “this is the first evidence that stiffness regulates these particular splicing factors,” said Reinhart-King.
Further study may investigate how to target alternatively spliced proteins in therapies and how changing mechanical cues can intervene and change how proteins are spliced. Also, by understanding how tissue stiffness influences specific protein changes, researchers may manipulate these properties to “elicit a certain program” for tissue engineering and rebuilding organs, Bordeleau said.
Co-authors included Sandra Shin, M.D., a researcher and pathologist at Weill Cornell Medical College who supplied patient breast tumor samples, and Robert Weiss, Ph.D., associate professor of molecular genetics at Cornell’s College of Veterinary Medicine, who provided mouse models for observing these processes.
The study was funded by the National Institutes of Health and the National Science Foundation.