Interventional Oncology as the Fourth Pillar of Cancer Care
This article, by David Li, MD, PhD, and David C. Madoff, MD, FSIR, FACR, first appeared in the Gastrointestinal Cancers Symposium Daily News.
In 2015, the Radiological Society of North America (RSNA) celebrated its centennial anniversary and reflected on a century of historical milestones, including “CT machine first displayed at Annual Meeting” and “interventional radiology emerges in Radiology” in 1972. According to RSNA’s timeline of milestones, the interventional radiology journal article, which documented elective arterial embolization as a method to control gastrointestinal bleeding, ushered in the establishment of interventional radiology, a field that “combined the acumen of diagnostic radiology with surgical skills.”
To commemorate the centennial, Radiology, the leading peer-reviewed journal in the radiology field, published a series of “Golden Oldies” each month in 2015 emphasizing 15 articles published in the journal that have changed the way each subspecialty practices. The October 2015 issue focused on vascular and interventional radiology. Articles included landmarks in vascular interventions, such as “Percutaneous Transluminal Treatment of Arteriosclerotic Obstruction” and “Selective Clot Lysis with Low-Dose Streptokinase” by Dotter et al., which documented some of the pioneering work that has developed into angioplasty and thrombolysis for peripheral arterial disease. Many of the highlighted articles served as the foundation for our current practice of interventional oncology, including papers that established both percutaneous ablation and transcatheter embolization as mainstay treatments for primary liver cancer.
Defining Interventional Radiology
Varying historical perspectives bring to light the question of how to define interventional radiology. Is a field that combines the acumen of diagnostic radiology with surgical skills sufficient as an encompassing definition by which we identify ourselves? The 15 articles emphasize a common theme in the nascent field of interventional radiology-—one of innovation that crosses all boundaries. Interventional radiologists have contributed to all fields of medical care, including the treatment of gastrointestinal bleeding and peripheral arterial disease, and the treatment of patients with cancer.
Our national societies have drafted a consensus “Global Statement Defining Interventional Radiology,” listing the core features:
- Expertise in diagnostic imaging and radiation safety;
- Expertise in image-guided, minimally invasive procedures and techniques as applied to multiple disease and organs;
- Expertise in the evaluation and treatment of patients suitable for the image-guided interventions included in the scope of interventional radiology practice; and
- Continual invention and innovation of new techniques, devices, and procedures.
As such, the core skills of an interventional radiologist translate incredibly well to the oncology field. Expertise in diagnostic imaging is critical to understanding the staging and resultant treatment algorithms for patients with cancer. Cancer is usually not confined to a single organ system, so the understanding of multiple organ systems is necessary for optimal management. As we continue to gain shared experience with our medical, surgical, and radiation oncology colleagues in multidisciplinary settings, such as tumor boards and shared clinics, we continue to gain expertise in the evaluation and treatment of patients suitable for image-guided interventions. Minimally invasive image-guided interventions are well suited for patients with cancer, many of whom have complex comorbidities that preclude them from undergoing surgery. Interventional oncology has developed directly from the robust role of interventional radiology in cancer care.
The subspecialty of interventional oncology has already gained traction in its field. Dedicated textbooks, such as Clinical Interventional Oncology: Expert Consult; Interventional Oncology: Principles and Practice; and Interventional Oncology: A Practical Guide for the Interventional Radiologist, are now all widely available to the general public. There are now several scientific meetings focused on interventional oncology, including the World Conference on Interventional Oncology, the European Conference on Interventional Oncology, and Synergy: A Multidisciplinary Approach to Interventional Oncology. As interventional radiology undergoes an educational shift toward increased patient-centric care with its integrated interventional radiology/diagnostic radiology pathway, the field of interventional oncology will only continue to strengthen.
Multidisciplinary Team Settings
Multidisciplinary team settings, such as tumor boards, remain one of the critical hallmarks for the growth of the field of interventional oncology. Through shared tumor boards and clinics, interventional oncologists are exposed to the knowledge and patient experiences critical in staying up to date on cancer care. The interventional oncologist’s role in the care of patients with cancer is best highlighted by the management algorithms for gastrointestinal carcinomas, particularly in the management of hepatobiliary carcinomas and colorectal metastases.
Case example
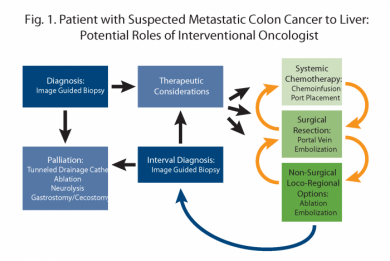
A patient who initially presents with colon cancer and suspected metastatic disease to the liver serves as an excellent model to highlight the increasing role of the interventional oncologist in cancer care, as depicted in Figure 1. Interventional oncologists serve as one of the initial points of contact for these patients, with the ability to perform image-guided biopsy to help with staging, diagnosis, and tumor gene status to guide therapeutic regimens and prognosis. Interventional oncologists are involved in early aspects of care, including chemo-infusion ports, to aid in systemic therapy administration. If the liver lesion is in a location requiring major surgery, such as an extended right hepatectomy, interventional oncologists can aid surgeons by performing portal vein embolization to increase functional liver reserve prior to resection. If there is localized recurrence after surgery, interventional oncologists can obtain tissue with repeat image-guided biopsy to check the evolving genetic status of the tumor. Interventional oncologists can also perform locoregional therapies, such as ablation or embolization, to aid in tumor control in this setting. Interventional oncologists also play an active role in the palliative care setting, with the ability to perform minimally invasive tunneled pleural and peritoneal drainage catheter placement, feeding/decompression gastrostomy placement, nerve blocks, and ablations to aid in pain relief and symptom control.
The Future
In celebrating its centennial, the RSNA has embraced the motto “Innovation is the key to our future” and is welcoming predictions for the next century of care rather than focusing on past accomplishments. Interventional oncologists remain on the forefront of technological advances. New technologies, such as irreversible electroporation and high-intensity focused ultrasound, provide novel treatment options for patients previously thought to be ineligible for local therapies. New imaging fusion techniques and electromagnetic needle navigation allow for greater precision in the delivery and monitoring of ablation devices. New catheters and wires allow for precise delivery of therapeutics directly to the vascular supply of tumors with minimal non-target deposition. Available therapeutic embolic agents now include drug-eluting beads and yttrium-90–labeled microspheres in addition to traditional vascular occlusion agents and chemotherapy regimens.
However, it is not from innovation alone, but through multidisciplinary collaborations that interventional oncology as a subspecialty continues to provide impactful care to patients. In keeping with this emphasis, recent RSNA historical milestones include “Patient-Centered Radiology Focus” and “Clinical Trials Methodology Workshop Debuts” in 2005 and 2006, respectively. Evidence-based, patient-centric care are critical cornerstones to our developing field. As such, interventional oncologists continue to be active participants in tumor boards and have also established outpatient clinics for consultation and follow-up care for patients with cancer.
Through robust collaboration with medical, surgical, and radiation oncologists, interventional oncologists continue to establish themselves as the fourth pillar of cancer care. Interventional oncologists are active participants in both the hepatobiliary cancers and colon cancer National Comprehensive Cancer Network guideline panels. In addition, multiple clinical trials have been initiated evaluating the role of transarterial therapies either as a primary treatment or in combination with either radiation therapy or systemic therapies for the treatment of both primary and metastatic liver cancers. Most importantly, interventional oncologists have the privilege of treating and learning from patients on a daily basis through shared multidisciplinary settings.
As interventional oncologists, we are excited for what the future brings. We continue to be grateful for our partners in innovation—medical, surgical, and radiation oncologists—and most importantly, for our patients, as we strive toward providing state-of-the-art, evidence-based, minimally invasive, patient-centric therapies as the fourth pillar of cancer care. We hope to rise to the occasion as an additional pillar of support to the increasingly complex multidisciplinary approaches required to treat patients with cancer in the 21st century.