Transforming Cancer Care
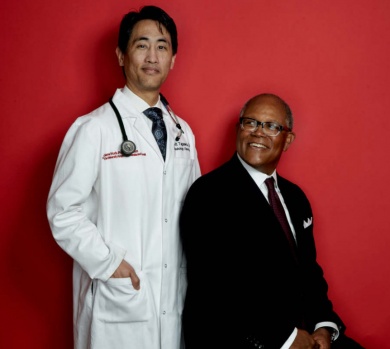
Williams’s oncologist, Scott Tagawa, MD, MS ′10, the Richard A. Stratton Associate Professor in Hematology and Oncology at Weill Cornell Medicine, enrolled him in a clinical trial, which involved combining chemotherapy with an experimental method of delivering a toxic payload "directly into the tumor cells, regardless of where they are," says Tagawa, a member of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine. For this to be possible, scientists had to harness a mechanism used by the immune system to find and suppress pathogens. They reprogrammed a protein that typically locates and neutralizes viruses or bacteria to instead seek out prostate cancer cells. They then attached a radioactive agent to it, which would be delivered directly into the cancer cells after the protein attached to its target, says Tagawa, an oncologist at NYP/Weill Cornell. For Williams, this cancer-seeking poison arrow, called a radiolabeled monoclonal antibody, "completely turned things around." Today, while he continues to see Tagawa once a month and regularly undergo treatment, his disease is more controlled—and chronic—than terminal, he says. "When I tell people I have cancer, it’s the last thing they would ever believe," Williams says. "Even my family forgets I’m sick sometimes."
Based on success stories like his, immunotherapy is now considered the "fifth pillar" of cancer therapeutics, joining surgery, radiation, chemotherapy, and precision-targeted therapeutics. While the latter four attempt to remove or attack cancer cells directly, treatments under the immunotherapy umbrella harness a patient’s own immune system to attack their disease from within. Today, scientists are making significant advances, offering patients with many types and stages of disease the chance of a lasting and dramatic remission.
But while there’s a lot of excitement about immunotherapy’s potential, these developments in no way mean that cancer will be rendered obsolete anytime soon. This is because, at least right now, only 10 to 30 percent of patients respond to these treatments, and in many cases, scientists don’t understand why. With more research and clinical advancements, experts think that instead of finding a cure for cancer, we’ll see more patients living with a controlled disease in the coming years, thanks in large part to immunotherapy. "Now that we have better surgery, less severe and more targeted radiation and chemotherapy, plus immune therapies, we are beginning to attack cancer in a scientific way rather than an empirical way," says Lewis Cantley, PhD ′75, the Meyer Director of the Meyer Cancer Center and a professor of cancer biology in medicine. "Our goal is to figure out how to combine these therapies for each and every patient so that we can control their disease and help them live a healthy, normal life. Immune therapy is not going to be a cure-all for all cancer, but it’s certainly going to be a remarkably good tool to use."
Cancer immunotherapy traces its roots to the early 1890s, when a surgeon infected patients with strep bacteria in the hope that they’d have a strong response that might eradicate their tumors.
Cancer immunotherapy traces its roots to the early 1890s, when New York-based surgeon William B. Coley, MD, infected patients with strep bacteria in the hope that they’d have a strong response that might eradicate their tumors. He had some success with this treatment, called "Coley’s toxins," but never fully understood why it sometimes worked and often did not. Over the years, other scientists pursued aspects of his approach, with little success. It wasn’t until scientists better understood how the immune system functions that they could research and develop smarter ways to use it to fight malignancies.
A major breakthrough in the field came from James Allison, PhD, now at MD Anderson Cancer Center in Houston. In the late 1980s, he discovered a protein called CTLA-4, which he found could inhibit the immune system’s ability to alert fighter T cells—known for their ability to track down and kill pathogens—of tumor cells in their midst. Rendered invisible to the body’s natural defenses, these tumor cells could multiply and thrive. Additional findings Allison made in the late 1990s led to the clinical development of the first-ever drug that blocks CTLA-4, thereby releasing the T cells’ brakes, so that these immune cells are unleashed on the disease. His work to develop this type of drug, known as an immune checkpoint blocker, won Allison the Lasker Award—America’s version of the Nobel—in 2015.
Immune checkpoint blockers are to date considered the most promising type of immune-based therapy. But scientists are studying other approaches as well. These include additional monoclonal antibodies, like the one used on Williams, which are programmed to find specific types of cancer cells and deliver medication directly to them; supercharged T cells, which are genetically altered in a lab to find tumor cells and tumor stem cells, and then multiplied into the billions before being infused back into the patient so that they can stage a massive attack; therapies to alter and engage the immune cell-rich area around tumors, called the microenvironment; and cancer vaccines, which would prevent the disease from developing in the first place.
Additionally, investigators are testing ways to combine immunotherapy with chemotherapy or radiation, and also studying how checkpoint blockers and other FDA-approved immunotherapy drugs might be used in earlier stages of the disease to produce the best outcome.
With new immune-based therapies and improved surgeries, radiation, and chemotherapy, death rates from cancer have dropped significantly in recent years. But doctors will still diagnose more than 1.6 million new cancers in the United States this year, and close to 600,000 people will die of the disease. Because only 5 percent of cancer patients will ever make it into a clinical trial, moving discoveries in labs into doctors’ offices is critical.
With new immune-based therapies and improved surgeries, radiation, and chemotherapy, death rates from cancer have dropped significantly in recent years.
Hope for Leukemia Patients
A promising form of immunotherapy involves the use of chimeric antigen receptor (CAR) T cells, which are genetically engineered to recognize a surface protein expressed on tumor cells. Currently, the T cells used in this type of treatment are taken from the patients themselves, a process that requires weeks of preparation before the cells are ready for infusion. Thus far, CAR T therapy has primarily been used in patients with acute lymphocytic leukemia (ALL); WCM has partnered with the drug company Cellectis to develop a form of the therapy for patients with acute myeloid leukemia (AML), the most common form of leukemia in adults. "Treatment with CAR T cells has shown impressive results in patients with acute lymphocytic leukemia, but the process of harvesting T-cells from sick leukemia patients can be logistically and clinically challenging," says Gail Roboz, MD, a professor of medicine. "We hope to be able to use T cells from healthy donors and engineer them to selectively attack CD123, an antigen present on AML stem cells."
Roboz, a member of the Meyer Cancer Center and an oncologist at NYP/Weill Cornell, is collaborating with scientists at Cellectis and with Monica Guzman, PhD, assistant professor of pharmacology in medicine, a leukemia stem cell expert. "Targeting stem cells in AML is important," says Guzman, "because most patients who go into remission relapse when the root of the disease—which can’t be killed by standard chemotherapy—allows it to rise again and again." Guzman, who developed the first antileukemia stem cell therapies twenty years ago during her doctoral work at the University of Kentucky, says that a particularly exciting part of the Cellectis project is the possibility of faster access to engineered T cells by using healthy donors to generate an "off the shelf" product. Says Guzman: "For AML, which is incredibly fast moving, speed is important." She and Roboz hope the T-cells will grow and proliferate when their target is present, but slow down and eventually "commit suicide" when their target is eliminated. "The project is using breakthrough technology," says Roboz, "and the results have been exciting."
‘Bridging the Gap’
Nasser Altorki, M.D., head of the clinical lung cancer program and the Gerald J. Ford–Wayne Isom Research Professor in Cardiothoracic Surgery, is considering two clinical trials that would test various immune-based approaches to treating lung and esophageal cancers. One of those would use immune checkpoint inhibitors on pre-surgical patients with early—instead of advanced—disease. Some would get these inhibitors alone, while others would get them with "a very tiny dose" of radiation therapy, says Altorki, a member of the Meyer Cancer Center. After the cancer is removed, investigators would be able to compare the changes that occur before and after treatment, in the hope of better understanding why only a small percentage of patients currently respond to these therapies and whether addition of a tiny dose of radiation improves the results. A similar investigation would look at patients with esophageal cancer, and compare those given immune checkpoint blockers and chemotherapy before surgery to others who get those treatments plus radiation. Again, the goal would be to find out why some patients respond when others do not. "Asking these questions is very important, because it allows us to bridge the gap between laboratory research and patient care," says Altorki, a cardiothoracic surgeon at NYP/Weill Cornell. "We hope to ask very specific questions that we believe would lead to an improvement of the treatment paradigm."
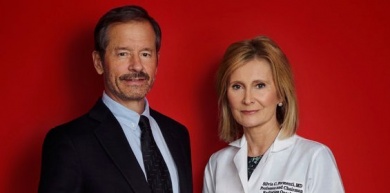
Tumors into Vaccines
A final—and next-generation—area of immunotherapy research at WCM is focused on seeing how immune-based approaches might be able to enhance other types of therapy. Silvia Formenti, MD, chairman of radiation oncology and the Sandra and Edward Meyer Professor of Cancer Research, focuses on immunotherapy paired with radiotherapy, and how the latter might help the former transform patients’ tumors into personalized vaccines directly at the site of their disease. Formenti says that a decade ago—before she arrived at WCM in April 2015—she started noticing that many of the effects of radiotherapy on tumors were in fact mediated by the immune system. "At that time, there were occasional reports in the literature that when a spot on the lung was treated with radiotherapy, the doctor would also see an effect far away—like in the liver," says Formenti, associate director of radiation oncology at the Meyer Cancer Center and radiation oncologist-in-chief at NYP/Weill Cornell. She thought this extremely rare occurrence might be caused by the immune system, which was somehow called to attention by the radiotherapy. From there she had an idea. "Maybe in some patients, when you irradiate one of the lesions, it will not only help the tumor respond and convene and kill some cells, but also acquire a memory that can be applied to regions away from the field," Formenti explains. "Somehow radiation will turn the tumor into a vaccine."
Targeting Pancreatic Cancer
Can immune suppression be reversed?
Douglas Fearon, M.D., the Walter B. Wriston Professor of Pancreatic Cancer Research, is considering a new clinical trial to test whether a drug called AMD3100 can reverse the immune suppression process at work in the pancreatic cancer microenvironment. Unlike many other cancer types, pancreatic cancer has shown no response to immune checkpoint blockers. This is because the immune suppression mechanism at play affects fibroblastic stromal cells in the tumor’s microenvironment, which then block T cells’ entry to the tumor region, rather than affecting the T cells themselves. In recent animal models, administering AMD3100 to overcome the block to T cell accumulation in pancreatic cancer has meant that the T cells can do their work and destroy the tumor. Based on this finding, gastrointestinal oncologist Tong Dai, MD, PhD, an assistant professor of medicine, and Manish Shah, MD, the Bartlett Family Associate Professor in Gastrointestinal Oncology—both members of the Meyer Cancer Center—are hoping to direct the U.S. component of a phase 1 clinical trial that has been initiated in Cambridge, England, to test the drug’s safety. This trial will determine whether the drug improves the tumor’s immune response by comparing a pre-treatment biopsy to one collected post-treatment. "If it works out and if we uncover this fundamental reason why tumors suppress an immune attack, I think we’d find some of the same characteristics in lung cancer, colorectal cancer, prostate cancer, and others," Fearon says.
Modulating the Microenvironment
Researchers attack a tumor’s habitat
CAR T cells are currently demonstrating impressive activity against liquid malignancies, but these engineered T cells have shown minimal effects in solid tumors due to the immunosuppressive strategies at play within the mass itself. "When you surgically remove an ovarian tumor from a patient, more than half the mass is made up of non-cancerous cells," says Juan Cubillos-Ruiz, Ph.D., an assistant professor of microbiology and immunology in obstetrics and gynecology. Known as the tumor microenvironment, this noncancerous material contains endothelial cells that provide blood to the tumor, stromal cells that secrete growth factors, and also immune cells—which, in ovarian cancer, can comprise up to 40 percent of the whole. So what are those immune cells doing there, and why aren’t they successfully attacking the cancer? "Because of several cancer-derived factors, these immune cells, which were the first responders and originally protective, are made dysfunctional and instead help the tumor grow," says Cubillos-Ruiz, a member of the Meyer Cancer Center. In recent years, it’s become clear that this process of turning immune cells pro-tumoral isn’t unique to ovarian cancer, but is also found in breast cancer, lung cancer, and other solid tumor types as well. That’s why Cubillos-Ruiz’s team is investigating new strategies to modulate the tumor microenvironment and harness the protective function of immune cells within it, which he calls a "Trojan horse" approach.
In ovarian cancer, a tumor’s toxic microenvironment modifies proteins located in the endoplasmic reticulum—the network of membranes that controls folding and secretion of proteins—which in turn triggers a transcription factor known as XBP1. Once it’s activated, dendritic immune cells, which would typically alert T cells to fight an intruder, are turned off, and the tumor can thrive without anything to slow its growth. This process, known as the ER stress response, might be controlled if nanoparticles containing a XBP1-silencing molecule are injected at the tumor site, Cubillos-Ruiz explained in a groundbreaking paper published in Cell last summer, with Dean Laurie Glimcher, MD, as senior author. Now, they’re trying to find out if the same process occurs in other types of cancer, while working to develop a potent inhibitor that could one day be used in patients to shut down that pathway. Says Cubillos-Ruiz: "A drug like that would be a double-whammy strategy against cancer."
Vivek Mittal, Ph.D., an associate professor of cardiothoracic surgery and of cell and developmental biology, is another scientist studying the role of the tumor microenvironment in mediating immune suppression in lung cancer. Mittal is identifying various modes that lung tumors use to elicit immune-suppressive pathways, and harness this information to tailor specific therapies to shut them down—which has led to combination immune therapies to hit the two or three most dominant pathways at the same time. Immunotherapies are also being combined with standard-of-care chemotherapy, radiation therapy, and targeted therapies. Because all of this knowledge is coming from the tumor’s microenvironment—not the cancerous cells themselves—it’s like looking at the entire galaxy in relation to how it impacts one planet, Mittal says. His studies rely in part on active collaborations with surgeons, who often remove a full lobe of the cancerous lung that includes not only the tumor nodule, but also adjacent normal tissue. "From the same patient, we can compare a normal immune cell to its counterpart inside the tumor, and can identify what is being activated and what is being suppressed," says Mittal, a member of the Meyer Cancer Center. "By finding out more about how specific immune cells under the influence of the tumors might be contributing to the cancer’s progression, we’re uncovering new potential targets for therapies."
Cubillos-Ruiz’s team is investigating new strategies to modulate the tumor microenvironment and harness the protective function of immune cells within it, which he calls a ‘Trojan horse’ approach.
‘From the same patient, we can compare a normal immune cell to its counterpart inside the tumor,’ Mittal says, ‘and can identify what is being activated and what is being suppressed.’
While this approach will only work in a minority of patients, the effect can be prolonged and dramatic, Formenti says. One patient, whom she calls "Mr. P," had metastatic lung cancer, which had spread to his liver and bones; he came to her in 2012 for palliative radiotherapy in his hip. Before his appointment, he’d stumbled upon a story about her research using radiotherapy with immune checkpoint blockers in mice and, ready to enter hospice care, he begged her to try it on him. After treating one small lesion that was nowhere near his lung, "literally everything he had—everything—went away," Formenti says. Today, he is still healthy and disease free, and has never had another treatment. Since then, she has run a study with patients like him, and found that one out of three patients respond to this treatment, which shrinks their tumors or stops them from progressing when they weren’t responding to chemotherapy. Now, she’s working with a $1.6 million grant from Bristol Meyers Squibb to combine two immune checkpoint blockers with radiotherapy in a trial to treat patients with metastatic disease and multiple tumors. She’s leading three additional clinical trials at WCM, each combining immunotherapy with radiotherapy, and is both the principal investigator on an NIH-funded project and the leader of a Department of Defense breast cancer research program focused on combining radiation and immunity. And she is also part of a new strategic, preclinical research alliance with one of the Janssen Pharmaceutical Companies of Johnson & Johnson to develop new treatment approaches for various types of cancer.
While Formenti pioneered this field, she is no longer alone: there are now eighty-one clinical studies in the country combining immune-based therapy with radiotherapy. "We’re in a huge immune-oncology revolution right now," she says, "and pharma is taking this on with the speed of light." But while there’s a lot to be excited about, Formenti says, there’s still a lot of work to be done. "We’re looking at more and more targets for immune checkpoints, and for each of them, we’ll have to figure out the best way to incorporate radiation," says Formenti, who is collaborating with cancer immunologist Sandra Demaria, MD, interim assistant professor of radiation oncology. "We’ll need to design trial after trial until we find the correct way to do it."
Indeed, researchers have much yet to accomplish, including establishing the correct doses and protocols. At the same time, the healthcare system must address the often-astronomical price tag of immune-based drugs, which can cost into the hundreds of thousands of dollars per year. Despite these challenges, physicians and scientists have high hopes for future breakthroughs. "Immunotherapy is something that has captured the imagination of doctors and patients for decades, and for the very first time, we now have immune-based treatments that are working," Altorki says. "Hopefully this new phase of immunotherapy is the first leg of a sustained ascent."
‘His Scans Look Great’
For one patient, a terrific response
Seventy-eight-year-old Stanislaw Sniarowski of Bay Ridge likely wouldn’t be alive today if not for an immune-based drug. A year ago, he was prescribed Opdivo to treat his stage IV lung cancer. Known as a checkpoint inhibitor, Opdivo works by reactivating T cells to detect and attack tumor cells, a response that his cancer had stunted. Opdivo received FDA approval in March 2015 for use in patients with advanced stage squamous non-small cell lung cancer after chemotherapy, and additional FDA approvals for similar immune-based drugs targeting lung cancer have followed. In the short time that these drugs have been commercially available, Sniarowski’s oncologist, Ronald Scheff, MD, says they’ve already made a big impact among the fifty or so patients he’s used them on. "Like a lot of treatments for lung cancer, only a certain number of patients are going to respond," says Scheff, an assistant professor of clinical medicine and a paid consultant to Bristol Meyers Squibb, which makes Opdivo. "But for those who do, they can respond for a very long time."
More than two years after diagnosis, Sniarowski is ‘back to doing normal activities,’ his oncologist says.
Sniarowski, who Scheff calls "one of our superstars," had multiple recurrences of his lung cancer, which had initially been removed surgically, and was too sick to do much on his third type of chemotherapy; then Opdivo hit the market. Now, more than two years after diagnosis, "his scans look great, he’s gained weight, and he’s back to doing normal activities," says Scheff, a member of the Meyer Cancer Center and an oncologist at NYP/Weill Cornell. Among those is dog-sitting his son’s German shepherd and taking regular weekend trips to the Poconos. "He’s not nauseated, there are no headaches—the treatment is like taking a vitamin shot," says his son, Mariusz Sniarowski. "Considering his condition and his age, he’s doing great."
This article first appeared in Weill Cornell Medicine.
Photos by Tiffany Walling/Getty Images