Targeting epigenetic switches may lead to novel therapies for B-cell lymphomas
Targeting epigenetic switches that have been linked to lymphomagenesis may lead to the development of new therapy options for B-cell lymphomas, according to a presenter at Lymphoma & Myeloma 2015.
Melnick provided three examples of this process and how they may be harnessed for targeted therapies.
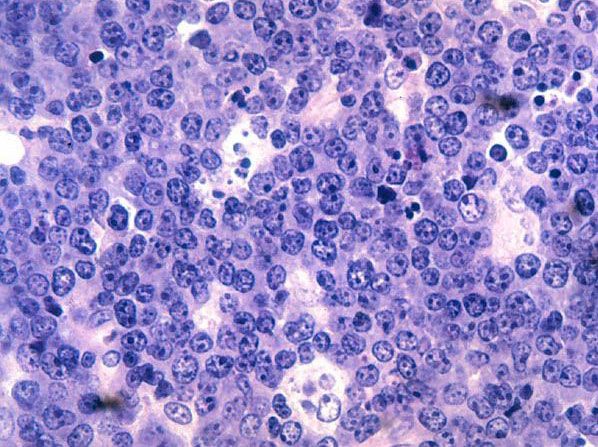
EZH2 represents a switch that suppresses B-cell promoters involved in terminal differentiation and cellular checkpoints, which is required for B-cells to form germinal centers during the humoral immune response. EZH2 is mutated in 30% of germinal center B cell type diffuse large B-cell lymphomas (DLBCL) and follicular lymphomas.
“Mutations in EZH2 cause it to become hyperactive and hence to keep gene promoters switched off. That causes an accumulation of germinal center B cells, which eventually transform to lymphoma” Melnick said. “You get these massive germinal centers because those B cells simply cannot exit the germinal center and differentiate into plasma cells — they get stuck in the germinal center stage.”
Drugs that specifically target EZH2 have completed phase 1 trials, Melnick said. However, who should receive this class of drugs remains a research question.
“The fact is that these drugs will likely be active in wild-type and mutant follicular lymphoma and DLBCL and we don’t have any biomarkers to indicate which patients would likely be sensitive or resistant to EZH2 inhibitors,” Melnick said. “A challenge moving forward with the phase 2 trials in this context will be trying to figure that out.”
BCL6 is another on/off switching controlling B-cell enhancers that appears mutated in 50% of patients with DLBCL. CREBBP and EP300 mutations may disrupt their ability to counteract BCL6 enhancer toggling, leading to enhanced repression of BCL6 target enhancers.
“The lucky thing is that we have compounds that can block the ability of BCL6 to suppress enhancers,” Melnick said. “If you treat lymphoma cells in vivo with these drugs, you get extremely powerful killing of lymphomas and even tumor eradication. It’s going to be a good way to counteract mutations that disrupt that particular switch.”
A third example is KMT2D, a switch that enables B-cell enhancers to respond to key B-cell signaling pathways. It is a tumor suppressor in B cells, without which mice develop lymphomas.
Research has shown that KMT2D depletion reduces cell death and gene activation in response to CD40 signaling in DLBCL cells.
Patients with KMT2D mutations may be less responsive to drugs activating CD40 to kill lymphoma cells and perhaps these mutations could serve as a biomarker for patients unlikely to respond to this therapy, Melnick said.
Each of these epigenetic switches show promise for therapeutic targets.
“The opportunity for us from the medical standpoint is that these are all switching mechanisms that can be targeted with the right kinds of drugs,” Melnick said. “If we can understand exactly how to do this medically, there is the opportunity to reverse the malignant phenotype of lymphoma cells to restore them to their normal path.”
This article first appeared in HemOnc Today. Read the original story here.