Taking the Next Step in a Storied Career
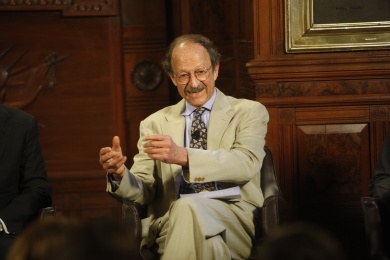
On March 31, 2015, Harold Varmus, M.D., left his position as Director of the National Cancer Institute (NCI) to join the faculty of Weill Cornell Medical College in New York as its Lewis Thomas University Professor of Medicine. Dr. Varmus was also named Senior Associate Core Member of the New York Genome Center, a newly formed consortium of 16 academic and medical institutions to use genomic methods to combat several diseases, including cancer.Douglas R. Lowy, MD, who served as Deputy Director of NCI under Dr. Varmus, became Acting Director of the agency on April 1, 2015.
In his nearly 5 years as head of NCI, Dr. Varmus steered the agency through turbulent times, including a government shutdown and a funding cut of 5.5%, which reduced NCI’s budget to $4.78 billion. Still, Dr. Varmus’ accomplishments during his tenure are notable, including the institution of the Provocative Questions initiative; the creation of the Center for Global Health and the Center for Cancer Genomics; the transformation of the Cooperative Group program into the National Clinical Trials Network; and the launch of a large new initiative to study tumors driven by mutantRAS genes, among others.
Dr. Varmus’ long association with the National Institutes of Health (NIH) began in 1968, when he studied bacterial gene expression with Ira Pastan, MD, who is now Co-Chief of NCI’s Laboratory of Molecular Biology. Dr. Varmus served as Director of the agency from 1993 to 1999. Before returning to NIH as Director of NCI in 2010, Dr. Varmus was President of Memorial Sloan Kettering Cancer Center in New York. Prior to his appointment to lead NCI, Dr. Varmus was named co-chair of President Barak Obama’s Council of Advisors on Science and Technology, served on the World Health Organization’s Commission on Macroeconomics and Health, and was Chair of the Scientific Board of the Bill & Melinda Gates Foundation Grand Challenges in Global Health. He is also a member of the National Academy of Sciences and the Institute of Medicine.
Recognized for his many contributions to the study of retroviruses and the genetic basis of cancer, Dr. Varmus was co-recipient with J. Michael Bishop, MD, of the 1989 Nobel Prize for Physiology or Medicine for their discovery of the cellular origins of retroviral oncogenes. In addition to the Nobel Prize, Dr. Varmus was the recipient of the National Medal of Science and the Vannevar Bush Award.
In his new position at Weill Cornell Medical College, Dr. Varmus will continue his research on lung adenocarcinoma and the cancer-driving mutations found in the disease in a laboratory he is establishing in the Sandra and Edward Meyer Cancer Center. He will also serve as Senior Advisor toLaurie H. Glimcher, MD, Dean of Weill Cornell.
The ASCO Post talked with Dr. Varmus about his tenure as Director of NCI, the future of biomedical research, and this next phase in his career.
Working Within the Budget Framework
When you became Director of NCI, the budget for NIH had been stagnant or on the decline for a decade and was reduced by an additional 5.5% in 2012. How were you able to overcome NCI’s funding restrictions and still accomplish your goals?
The past 5 years have been very productive ones. Despite the declines in our budget, we’ve made a lot of good changes at NCI and done a lot of interesting things. I wish the budget was rising rather than falling, so we could have done even more, but that didn’t rule my everyday life while I was Director. We have to remember that NCI still has a budget of about $5 billion. The agency has a public responsibility to use those monies well, and that’s what I tried to do during my tenure.
There’s always a lot of justifiable complaining about a declining budget. I’m perfectly happy to say repeatedly that Congress needs to pay attention to the fact that NCI has $177 million less this year than it had the year I became Director. Even if we got the President’s full request for a 3% increase this year, NCI would still not be back to where it was the day I walked into the office. And although that is not good news, I just considered it to be the lay of the land and tried to work within the budget framework.
Despite funding constraints, we started a lot of new and interesting programs, including two new centers, one for Cancer Genomics and one for Global Health. I didn’t invent the idea of NCI working abroad; NCI has had programs in developing countries for many years. What I tried to do was to bring a sense of coordination and purpose to these programs.
We also attempted to improve the grant-making process in several ways. For example, we are engaging our scientists in identifying inadequately studied but important questions about cancer and providing grants to researchers to answer these questions. At the same time, we are maintaining the numbers of NCI’s traditional research project grants. We revitalized the cooperative clinical trials system—now called the National Clinical Trials Network and the NCI Community Oncology Research Program—to adapt to the advent of targeted drugs and immunotherapies and to enhance the contributions of community cancer centers. And we launched a large new initiative at the Frederick National Laboratory for Cancer Research to study tumors driven by mutant RAS genes.
Improving the Treatment and Control of Cancer
Over the next 5 to 10 years, what is one hopeful scientific/clinical area of research that you predict will lead to a major improvement in the outlook for patients with cancer?
I try to avoid predictions, especially about a time scale for improved care. However, I think there are things that look especially promising and require bigger investments at the moment, such as targeted therapies carried out with drugs and antibodies, based on our deeper understanding of carcinogenesis. There are still lots of problems; for instance, the genetic profile of a cancer is extremely complex, and we don’t often know what makes cells drug-resistant. Also, we haven’t learned how to give combination therapies effectively and don’t have optimized preclinical models for testing combination therapies. In addition, clinical trials to test new therapies need to be redesigned; NCI is now doing that with MATCH and similar trials.
Another area that is promising therapeutically is immunotherapy. I don’t mean just one kind of cancer immunotherapy but those that use antibodies fused to toxic proteins, genetically engineered T cells, and (perhaps most promising) immune checkpoint inhibitors for many types of cancer.
I’m encouraged by the fact that as more cancers are analyzed genetically, we are learning some important clues about why some people respond to immune treatment and others do not. So, I think that we will soon have a much better idea of the patients in whom immune therapies should be used, which ones should be used, whether they should be used in combination with conventional chemotherapy or with targeted therapies, and when in the course of an illness immunotherapy should be performed.
Everyone is passionate about finding therapies to cure cancer. I understand that and feel the same way, but our greatest gains are often made with the least fanfare in the prevention domain. Early detection also shows promise for certain cancers and perhaps less for others, but there are some opportunities here that are not being as actively pursued as I’d like to see. And certainly more widespread use of prevention strategies that are already at hand, most obviously the human papillomavirus vaccine for the prevention of cervical cancers and others, would be beneficial. It is less dramatic to protect someone from getting a cancer than it is to turn around late-stage metastatic disease, and we need to raise public awareness of the efficacy of prevention.
Biomedical Research
Given the current funding climate, what advice do you have for young investigators interested in pursuing a career in cancer research?
We are currently in a very difficult situation in the biomedical research ecosystem. We have a Malthusian dilemma: The longstanding assumption that the biomedical research system in the United States will expand indefinitely at a substantial rate has created a crisis. Some colleagues and I have been writing about the issue, and we are actively working on solutions to the problems we discussed in our article.1
We are creating a lot of scientists. That’s a good thing except we can’t accommodate them all in the traditional academic environment. At this point, someone being trained as a biological scientist interested in disease and human biology has about a 1 in 10 chance of becoming an academic principal investigator.
So, although the goal is still to attract the best people to consider careers in this field, because the work is incredibly exciting, they should be aware that there are a lot of things that can be done with a PhD in biology and that the chances of becoming an academic scientist aren’t high overall.
I could not be more enthusiastic about the scientific opportunities to do great work. But I think people need to go into biomedical research with their eyes open to the competition for jobs and funds and should know that the ability to work productively in this incredibly exciting field is not going to be available to everybody.
Happy to Be Back in New York
Please talk about your new positions as the Lewis Thomas University Professor of Medicine at Weill Cornell Medical College and Senior Associate Core Member of Weill Cornell’s New York Genome Center.
About 20% of my time will be spent working in the New York Genome Center. My role there is to facilitate the use of genomics in medical care by offering services to all cancer care providers throughout the New York area. The Genome Center is focused on driving scientific research to improve clinical care, and it is important that this new area of genomics is coordinated in New York, where there is a very strong research base. The rest of my time will be devoted to running my small laboratory group, teaching, and interacting with other faculty members at the Meyer Cancer Center, which is led by my good friend Lewis C. Cantley, PhD.
I think this is going to be a very enjoyable place for me. In addition to my work, I’ll be near all my buddies at The Rockefeller University and Memorial Sloan Kettering Cancer Center, both of which are just across the street. And my wife and sons are here, so I’m enthusiastic about being back in New York